The risks of severe complications during pregnancy, childbirth or postpartum can vary drastically depending on where the person lives, a new study suggests.
Among people with Medicaid insurance in the United States, rates of severe maternal morbidity – life-threatening complications during pregnancy, delivery or after childbirth – range dramatically from about 80 cases for every 10,000 live births in Utah to more than 200 per 10,000 in the District of Columbia, according to the study published Thursday in the journal Obstetrics & Gynecology.
That means rates of severe complications were about 2.5 times higher in DC than in Utah.
“We expected some variation at the state level. We didn’t necessarily think it was going to be a three-fold difference. So that was a pretty striking finding,” said lead study author Dr. Lindsay Admon, an assistant professor of obstetrics and gynecology at the University of Michigan Medical School and obstetrician-gynecologist at U-M Health Von Voigtlander Women’s Hospital.
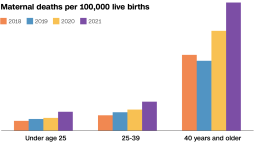
In the United States, attention is growing on maternal death rates and the fact that the nation has the highest rate of mothers dying in pregnancy or childbirth than other high-income countries. Just last month, data from the US Centers for Disease Control and Prevention revealed that the rising US maternal death rate climbed significantly yet again in 2021, reaching 32.9 deaths per 100,000 live births, up from 23.8 in 2020.
But maternal morbidity remains a public health issue too, Admon said.
“Maternal morbidity is 70 times more common than mortality,” she said. “These are severe adverse events as well, and I think these are the first time we’ve really had broad scale data at the state level about what the leading factors are in individual states.”
Where severe maternal morbidity is highest
The study authors – from the University of Michigan, Boston University, Columbia University and the University of Minnesota – analyzed Medicaid data on 4.8 million live births across 49 states and Washington, DC, from 2016 to 2018. They examined overall and state-level rates of severe maternal morbidity, occurring within 42 days before or after delivery.
“The data that we were able to put together reflects nearly half of all births occurring during the study period,” Admon said. Medicaid finances 41% of births in the United States.
The data showed that the overall rate of severe maternal morbidity among pregnant Medicaid patients, that did not involve blood transfusions, was 146.2 cases for every 10,000 deliveries – and those rates ranged depending on where the person lived.
The five states with the lowest rates of severe maternal morbidity, according to the data, were Utah, with a rate of 80.3 per 10,000; Maryland at 81.3; Rhode Island at 84.4; Nebraska at 88; and New Hampshire at 91.1.
The jurisdictions with the highest rates were Washington, DC, at 210.4 per 10,000; California at 190.5; Nevada at 187.1; New Jersey at 180.6; and New York at 174.6.
The most frequently identified cause of complications for patients was eclampsia, a serious condition involving high blood pressure during pregnancy, which can lead to seizures. Other leading causes of complications were acute respiratory distress in which fluid collects in the lungs, abnormal blood clotting and sepsis, a serious complication of an infection.
“For states where sepsis or severe infection is a leading indicator of maternal morbidity, an intervention might be to really focus their resources on early treatment of sepsis, on patient and community awareness of what sepsis is, and what the signs and symptoms are to look out for to seek care,” Admon said.
“In many states, eclampsia, which is a severe complication of hypertension in pregnancy resulting in a seizure, was a leading cause of morbidity, and in those states, I would hope that folks would think ‘OK, we really need to educate our population, our clinicians about hypertension in pregnancy,’ ” she said. “We know that complications from chronic conditions are the leading causes of maternal morbidity and mortality, and individuals in the US have been giving birth at older ages – with more chronic conditions, with more severe chronic conditions – for the last couple of decades.”
‘There’s a huge racial disparity’
The types of complications that can happen during pregnancy or childbirth also appeared to vary when the data was analyzed by race.
“When we looked at the leading causes of morbidity among the Black and White populations among Medicaid beneficiaries, basically, eclampsia was leading among the non-Hispanic Black population and sepsis among the non-Hispanic White,” Admon said. However, Black patients still had a higher rate of sepsis than White patients.
“There are six things that occur at higher rates among the non-Hispanic Black population,” Admon said: eclampsia, heart failure, acute kidney failure, respiratory distress, sepsis and disseminated intravascular coagulation, which causes blood clotting.
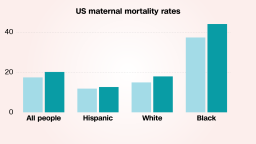
In states where race and ethnicity data were available, the researchers found that the overall rate of severe maternal morbidity was 2.1 per 100 live births among Black patients with Medicaid, compared with 1.3 per 100 live births among White patients.
“The research really highlights that we have a long way to go still towards achieving maternal health equity in the US,” Admon said. “I think it’s structural racism and that there’s a great deal of implicit and explicit bias that happens with health care, and those are really important issues that we need to tackle.”
The findings came as no surprise to Dr. Zsakeba Henderson, senior health adviser for the nonprofit National Institute for Children’s Health Quality in Boston, an expert on maternal and infant health inequities.
“The main reason why I’m not surprised is that we already know that there are significant racial and ethnic disparities in maternal morbidity and mortality in our country, with Black women three to four times more likely to die from pregnancy-related causes,” said Henderson, who was not involved with the new research. “And the main disparities that we see in mortality, we also see in morbidity.”
In other words, the factors behind racial disparities seen in maternal mortality could be some of the same factors driving state-by-state differences in severe maternal morbidity rates.
For example, the area with the highest morbidity rates in the new study was Washington, DC. According to a report released last year by the DC Maternal Mortality Review Committee, nearly all of the pregnancy-related deaths in DC – 90% – were among Black mothers, even though they constitute roughly half of all births there.
“So to see that DC had the highest morbidity was not surprising to me at all,” Henderson said.
“We can’t deny the fact that there’s a huge racial disparity, and so I suspect that states that have higher populations of Black pregnant moms, who tend to have a higher risk of morbidity and mortality, are likely to have higher numbers of severe morbidity,” she said.
The new findings can help guide discussions around what needs to be done to reduce rates of maternal morbidity in the United States, as well as the disparities by state and race, said Dr. Sarosh Rana, section chief of maternal-fetal medicine at the University of Chicago Medicine, who was not involved in the new study.
“It’s nice to have this data for people who are policymakers at the level of the state but also physicians and institutional leaders like myself. This data will help guide implementation of quality improvement initiatives and provide equitable care,” Rana said.
The new study is “eye-opening” and “can begin to inform clinical care, quality improvement, and policy change with regard to maternal morbidity and mortality,” Dr. Doee Kitessa, a general obstetrician and gynecologist at the University of Maryland Medical Center and an assistant professor at the University of Maryland School of Medicine, said in an email Thursday.
“This study can help hospitals and states target quality improvement initiatives toward the leading indicator of severe maternal morbidity,” said Kitessa, who was not involved with the research.
“While the data is based on billing codes and not patient charts, it’s an excellent start to understanding the causes of maternal morbidity by state and the disparities that exist,” she said. “This can help states and healthcare institutions begin to address and work to decrease the rates of severe maternal morbidity that are affecting the patients they care for.”
‘It is important to listen to patients’
Some policies have been introduced to tackle the United States’ maternal health crisis. At the federal level, the Black Maternal “Momnibus” Act of 2021, a sweeping bipartisan package of bills, aims to provide pre- and post-natal support for Black mothers, such as by extending eligibility for certain benefits postpartum.
Yet within individual health care systems, it’s important for physicians and leaders to pay attention to disparities in obstetrical care, Rana said, and among other factors that can lead to disparities, a key component is implicit bias in the care of Black women.
Get CNN Health's weekly newsletter
- Sign up here to get The Results Are In with Dr. Sanjay Gupta every Tuesday from the CNN Health team.
“I think it is important to listen to patients when they raise concerns and for expecting mothers to be aware of the signs and symptoms of pregnancy or childbirth complications. There are actually lots of signs that doctors should be talking about and that patients should be aware of,” Rana said, adding that common warning signs of preeclampsia and eclampsia, for instance, are headache, blurred vision, nausea, vomiting, abdominal pain and swelling of the hands or face.
“What I feel is, sometimes there’s a gap between a patient complaining and the doctor listening. There is so much data showing that patients, especially African American Black patients, are not always listened to,” she said. “That’s another barrier that a lot of our patients face, and it contributes to racial disparities.”