Government records reveal how supply shortages, lapses in care, a lack of transparency and inadequate infection control precautions are fueling the spread of Covid-19 within America’s nursing homes.
Troubled facilities and highly rated nursing homes alike have been struggling, with overwhelmed workers trying to identify, isolate and treat patients with the disease on top of their already demanding jobs. Measures aimed at protecting residents from the spread of the disease, meanwhile, have left them even more vulnerable and closed off from the public.
As a result, government watchdogs say it is becoming easier for substandard care to go unchecked and for some facilities to keep dangerous secrets.
“There are no tests,” a nurse at a Michigan facility told a state health department employee at the end of March, according to a government report, recounting how they were expected to take care of a unit full of pneumonia patients known as the “Covid unit” and had brought their own medical supplies for residents. “I have one (resident) who is actively dying right now.”
After announcing its first positive case of coronavirus, town officials in Massachusetts publicly condemned a local nursing home when the fire chief noticed a spike in calls from the facility but couldn’t find out what was going on inside the walls.
Police reports obtained by CNN through a public records request show how there had been warning signs about trouble brewing within a massive New Jersey long-term care facility — including multiple calls to police and reports of alleged patient neglect — for days before police discovered more than a dozen bodies in a makeshift morgue.

Many of the country’s nursing homes were already understaffed and frequently cited for lax infection control before coronavirus began to spread. Now staff are risking their own health and often lacking access to the supplies and testing they need as they care for a population at high risk of dying from the disease.
State long-term care ombudsmen, who are tasked with protecting residents, told CNN there are not enough eyes on these facilities at a time when oversight is needed the most.
Routine health and safety inspections have been suspended by the federal government to protect against any additional exposure to workers and residents. A CNN review of more than 100 inspection reports documenting visits still taking place, and complaint information gathered from state ombudsmen, provides a snapshot of serious problems during this pandemic — including unacceptable care and failures to take steps to stem spreading infections.
Families, who are often the ones keeping tabs on their loved ones’ care and in some cases even supplementing that care, have been restricted from visiting facilities in an attempt to slow the spread. CNN spoke with family members of nursing home residents in four different states who said they had struggled to get them tested for the virus or receive any updates about their conditions — and in some cases facility officials had kept vital information from them. One woman said she resorted to calling 911 herself to get her very sick father, who she said tested positive for coronavirus, admitted to the hospital — where she said he remained as of Thursday in critical condition.
On Sunday, the federal government announced a new rule requiring nursing homes to report Covid-19 cases to residents and their families and the CDC. Ombudsmen say it remains to be seen how — and how aggressively — this will be enforced by state inspectors. And even when facilities are cited for severe violations, critics have long argued that government penalties are too low to discourage the worst behavior.
“I’m concerned about neglect, poor care, rights being violated and abuse right now,” said Patricia Hunter, the long-term care ombudsman for Washington state, where the first nursing home outbreak publicly unfolded.
Repeated calls
More than a week before the Andover Subacute and Rehab Center II in New Jersey made headlines with the discovery of 17 bodies in the facility’s morgue on April 13, there were signs of a deepening crisis, according to police reports obtained by CNN.
Repeated calls to police were made. There were calls about patients with symptoms such as a high fever or respiratory distress. One resident was taken to the hospital, reports show; another call was cancelled even though the patient had been in “full code” – meaning they were in need of resuscitation. It’s unclear if a third ever made it to the hospital. Police also responded to a fire alarm there, but when they arrived, the report states, they were told it was a false alarm and that maintenance had it under control.
And three days before the bodies were found, reports show county health officials told police they had been fielding complaints about understaffing, a lack of protective equipment and patient neglect — including allegations that some residents weren’t being fed.
Even after the police discovered the extent of deaths at the facility (which they said at the time weren’t necessarily all linked to Covid-19), frantic calls to police continued. A resident said he wasn’t being allowed to call his family, though staff claimed to police it was because it was after hours. Other callers said the facility was in desperate need of more protective gowns and body bags, and a state senator reported there was no staff at the facility. One resident was sent to the hospital with hypothermia when the facility’s heat reportedly stopped working, a report shows, though staff later told police the heat was working. As public scrutiny intensified, a nurse reported receiving threats.

The state has since said more than 30 of the facility’s residents have died of Covid-19 and there have been more than 100 confirmed cases.
The facility owner said in a statement that staff had notified state authorities when “there was a tragic surge in patient deaths,” with 15 patients dying in a matter of days. He said employees tried to work with funeral homes to transport the deceased residents but were “left to manage these fatalities as best they could.” He added that resident safety was paramount at the facility, which had faced challenges related to a lack of protective gear and staffing complications after workers also became ill.
In an earlier statement, a facility attorney said that nursing home officials were confident that any future review by the state of what had occurred “will confirm that the facility has been addressing the unprecedented challenges from this pandemic appropriately.”
New Jersey has become a Covid-19 hotspot, reporting more than 2,500 confirmed and suspected deaths and more than 13,000 cases in hundreds of state long-term care facilities.
Another New Jersey facility with a high number of coronavirus cases is the Lakeland Health Care Center, where Denise Jorgensen’s 78-year-old father had been rehabbing a broken hip. She said she and her brother were kept in the dark about her father’s fever for days. It was around then a doctor told them he suspected their father had Covid-19 but the facility had run out of tests, according to the family. They said they only learned there had already been deaths in the facility when a mayor wrote a letter to borough residents saying there was a “major Covid-19 outbreak” and that eight residents had died of Covid-19.

Jorgensen said she couldn’t get through to anyone at the facility until 2 a.m. and was told not to be upset about the letter. She said around eight hours later, she learned that her dad had passed away. A facility official said he could not comment on specific individuals but that the facility has been “fully transparent in our reporting to state and local officials, accepting of their input and compliant with their recommendations.”
While state data shows there have been 19 Covid-19 deaths at the facility, borough documents tracking coronavirus at the Lakeland nursing home report 21 deaths specifically from the disease but say that 35 residents have died. On the day Jorgensen’s father passed away, there is a note in the borough’s records saying there were no test kits available.
“I don’t know what is going on in these nursing homes, but they are not being truthful with the families,” she told CNN. “And since we can’t visit or get in touch with anyone they are getting away with it.”
‘It feels horrible’
An analysis of the limited nursing home inspections that have occurred nationwide since last month shows failures in care may have caused Covid-19 to spread to both staff and employees. The reports detail supply shortages, failures to report Covid-19 infections and exposure to authorities, nurses not adequately monitoring potential symptoms of the disease and staff not properly wearing masks.
The Centers for Medicare & Medicaid Services, the federal agency that regulates nursing homes, instructed state officials in March to stop conducting routine health and safety inspections in order to protect residents. Instead, they have focused on inspecting facilities to check for infection control measures and investigate reports of “immediate jeopardy” situations — which CMS defines as meaning residents are at risk of serious injury or death.
In a review of recent inspection reports and enforcement letters obtained from the agency, CNN identified seven nursing homes that had been cited with the most serious violations related to Covid-19. Around 100 facilities had been cited for “deficiencies” specifically related to infection control since March 14, according to a separate spreadsheet provided by CMS.
At the Advantage Living Center in Roseville, Michigan, for example, a federal inspection report from the end of March recounts a litany of missteps. In one case, a nurse working the night shift found a patient who was “gray, kinda pale” and rapidly declining, saying that no one had given the resident the fluids they were supposed to have received. “Their mouth was so dry, they couldn’t even talk,” the nurse said. They then transferred the patient to isolation.
When the inspector asked why this resident with Covid-19 symptoms wasn’t transferred to the hospital sooner, the assistant director of nursing replied that the staff was overwhelmed. “I mean, they are taking care of so many people.” One nurse said the patient’s deteriorating condition hadn’t been better documented because the facility had been short staffed and very busy and most likely forgot, the inspector wrote.
Related coverage:
The resident later died at the hospital. Though they were still awaiting test results, doctors told the family they suspected it to be related to Covid-19, according to the report.
The inspection report documenting the patient’s care detailed other problems at the facility. Nurses reported bringing in their own medical supplies to treat residents, such as thermometers and blood pressure cuffs because the home didn’t have what they needed. The report also found inadequate monitoring of patient conditions, understaffing and failing to properly isolate residents with suspected Covid-19 — with a delay as long as nine days.
“It feels horrible,” a nursing assistant reportedly told the inspector when asked about whether staff were able to meet the needs of residents.
The Advantage Living Center did not respond to a request for comment from CNN, but provided a plan of correction in the inspection report — without admitting to the allegations made. It said that medical records showed the resident received fluids at the time they had been ordered and that employees have been retrained on a number of practices such as proper PPE usage. The facility said it had utilized temporary staffing and that facility-provided medical equipment was being used. Employees were also being “re-educated on Covid-19 as information emerges and trends are identified, including the rapid change in condition and rapid deterioration that can occur for residents with symptoms.”
‘We can’t trust them’
Born during the 1918 flu pandemic, 101-year-old Jean O’Brien’s health had already begun to decline as she struggled with the social isolation of being stuck in her room at the Four Chaplains Nursing Care Center in Westland, Michigan.
Family members worried that the virus would be a death sentence if she caught it, but fortunately — as far as they knew as of early April — there hadn’t been any coronavirus cases in the facility yet.

Then her daughter, Megan O’Brien, said her family learned from nurses on April 11 that the nursing home would be opening its doors to Covid-19 patients. O’Brien, her eight siblings and many nieces and nephews rallied together to call employees at the facility and its corporate owner, as well as government officials — demanding more information about how residents would be kept safe.
At that time, her biggest concern was the virus entering — and then spreading throughout — the facility. But she soon learned it already had. After appearing on the local news, O’Brien received an alarming message from Trace Fryz, whose mother was also at the facility. Fryz’s mother had tested positive for Covid-19 and died from the disease at a hospital weeks earlier. Fryz told O’Brien that it appeared the facility had not been forthcoming about Covid-19 deaths.
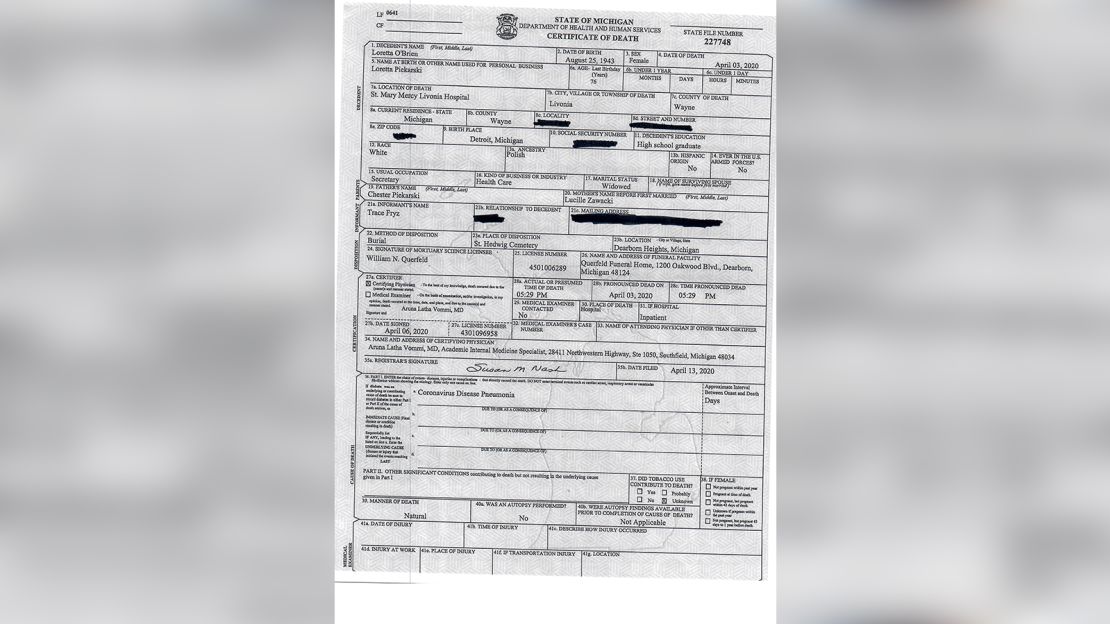
In an interview with CNN, Fryz said she first learned that her mother’s facility had multiple coronavirus cases from an ER doctor treating her mother when she was rushed there after falling unconscious at a dialysis appointment.
O’Brien said the facility continues to deny it has had any deaths related to the disease.
After finally getting her mother tested, with the help of separate hospice employees, O’Brien said the family learned on Tuesday that her mother had tested positive. They had been preparing to pull her from the home and care for her in a local Airbnb, and the family is now trying to figure out how to proceed, saying there have just been “too many lies from the facility.”

“We can’t trust them,” she said, adding that she is angry at the facility’s corporate owners, not its workers who she believes are still trying to take good care of her mother. “We would have taken her out weeks ago.”
The administrator at Four Chaplains told CNN that all she could say was that the facility was not accepting new Covid-19 patients. She referred all questions to its corporate owner, NexCare Health Systems, which did not respond to repeated inquiries. The state department of health said it had only just begun to collect data on Covid-19 deaths in nursing homes and suggested contacting the local health department. A Wayne County spokesperson told CNN that the facility currently has four Covid-19 deaths and 32 cases entered in a state database but said he would be unaware of any deaths where a resident hadn’t been tested for the disease.
‘Ticking time bomb’
As the virus has spread across the country, government watchdogs have been logging complaints from families, residents and employees about issues similar to those detailed by federal inspection reports.
In addition to the many reports of understaffing, PPE shortages and a lack of transparency, state ombudsman offices told CNN they have received complaints about patients being unfairly evicted and concerns from nursing home employees who have reported being worried they will be punished for speaking out about problems.
“Our program has been inundated with calls,” said Salli Pung, the Michigan state long-term care ombudsman, adding that she received more than 200 calls related to Covid-19 in March alone. “We continue to be very concerned about the overall lack of oversight in nursing homes and other long-term care facilities.”
Several offices noted concerns that nursing homes were not being forthcoming with information about Covid-19 cases in their facilities.
Advocates for long-term care residents said there is a short-term financial incentive to downplay infections since a publicized outbreak could result in families removing their loved ones and hurt future business. An outbreak could also open the doors for inspectors to cite a facility for numerous other violations such as understaffing.
In Virginia, state ombudsman Joani Latimer said one family member recently told her office that a nursing home resident had worsening Covid-19 symptoms but was not being tested or sent to the hospital. So the family member pulled the resident from the facility and drove them there, and a test came back positive. The family is now attempting to provide care at their home, Latimer said.

She said that the unraveling of nursing homes under the stress of a pandemic like this was a “ticking time bomb,” given the staffing crisis that already existed in long-term care facilities. “Until we fully examine and address that problem, we put our residents at risk.”
Hunter, the Washington state ombudsman, has had the opposite problem when it comes to complaints. During more normal times, the office’s phone rings around 50 to 80 times a week, with callers reporting dangerous situations within facilities or other problems that warrant further investigation, among other calls.
But now, as visits from family and local watchdogs that often lead to complaints have been mostly cut off, her office has only been getting around 25 calls a week.
“I have never witnessed the phone go silent and that is virtually what has happened,” said Hunter, who has been the state ombudsman for more than eight years.
‘Sudden rush of patients’
Scott Wodzinksi, the fire chief in the 10,000-person town of Littleton, Massachusetts, began noticing a sharp uptick in calls for service at the Life Care Center of Nashoba Valley at the end of March — reporting that his department had responded to the facility 18 times in a week.
Suspecting coronavirus could be the culprit, he and other town officials who were attempting to respond to the crisis and keep tabs on the situation say they were stonewalled when they tried to get answers from the nursing home. They wanted to know how many of its 100 or so residents were sick with the virus — information that was vital for the first responders.
A public controversy ensued, with the town claiming the facility initially turned down the help of the National Guard — which had been summoned in early April to conduct testing and ended up being let into the facility a couple days later.
The town asked the state health department to intervene. And with the help of lawmakers, they then sent a letter to the corporate owners of the facility, Life Care Centers of America, the same company that owned the nursing home in Kirkland, Washington — the site of the nation’s first outbreak. The Kirkland facility faces a federal fine of more than $600,000 for alleged failures if it does not correct the problems found. The town’s letter criticized the company for its “apparent lack of readiness or responsiveness to the COVID-19 threat” and stated that in both cases, administrators “did not provide adequate notification to authorities.”
Tim Killian, a crisis management spokesman hired by Life Care, said the company is confident that both the Nashoba Valley and Kirkland facilities had been in complete compliance with state and federal regulations. He said the company had hoped the federal government would have recognized that what happened in the Kirkland facility was “a unique situation.” About the Nashoba facility, he said the company shared the town of Littleton’s concerns but had been in touch with local and state health officials as soon as a positive test was received — adding that Life Care had welcomed the help of the National Guard.

“To us it’s this unfair environment where the public has somehow come to believe that nursing homes are to blame, that this was caused by us and not something that happened to us,” he told CNN, noting how facility workers had now been receiving death threats. “It was probably inevitable that Covid was entering our building as it has entered most nursing homes.”
CMS said an investigation at the Life Care Center of Nashoba Valley is ongoing and could not comment further. As of April 13, the most recent data provided by the facility, the majority of its residents tested positive for Covid-19 and there had been 14 deaths.
Do you have anything to share about Covid-19 in nursing homes? Is there something else you think we should investigate? Email us: [email protected].


























